Why mental health coverage is still a struggle for employer-sponsored plans
Insurers are still not doing a good job of covering behavioral health care services, a new report claims, which is limiting access for patients in employer-sponsored plans.
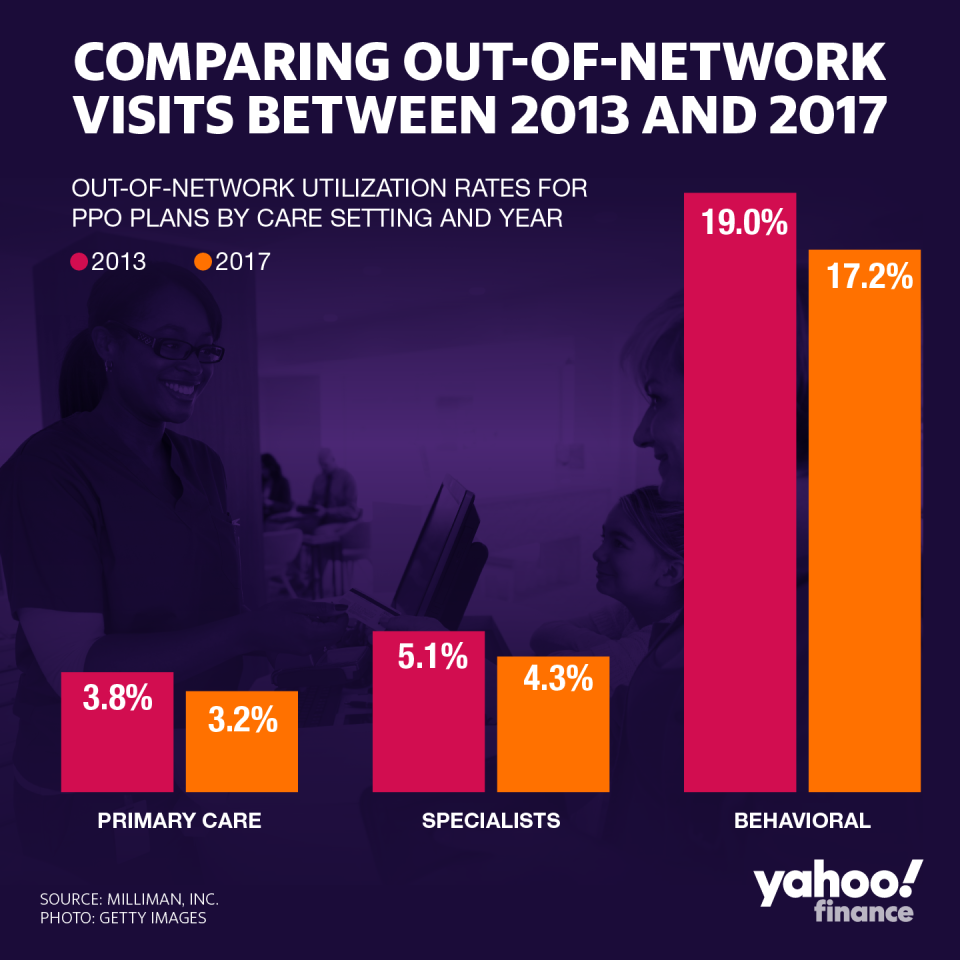
The 140-page report by Milliman, Inc., which was commissioned by a behavioral health group, found that patients are visiting out-of-network behavioral health providers at an increasing rate to obtain necessary treatment.
Some experts say behavioral health has long suffered in funding and attention, due to the stigma attached to seeking professional counseling — and therefore has always suffered from lower reimbursement rates when compared to medical doctors. Also, the status quo is a barrier to behavioral health professionals entering insurance networks.

Milliman found that both in-patient (being admitted to stay at a facility) and outpatient (leaving home the same day as treatment) care has skyrocketed by 85% and 90%, respectively, compared to 2017. Clients continue to choose out-of-network providers at a much higher rate than primary care or specialists, in large part because many providers are lacking in in-network options.
The data refreshes a similar report issued in 2017, and suggests the lack of mental health coverage is worsening — and likely to push up health care costs.
“The insurance companies are still playing yesterday’s game,” Patrick Kennedy, a former Democratic Congressman from Rhode Island who’s now a mental health advocate, told Yahoo Finance in an interview. He added that the report’s findings were unexpected.
Some industry observers maintain that insurers are unable to quantify reimbursements for behavioral health providers in the same way they do for other areas of health care — something Kennedy has sought to address with his 2008 legislation to put mental health coverage on par with standard medical care.
Industry players have made strides to rectify the situation. The Association of Health Insurance Plans, a national trade group representing insurers, told Yahoo Finance insurers have taken the challenges of behavioral health into account.
“If an in-network provider is not available, health plans do cover out-of-network care as in-network,” an AHIP spokesperson said.
“They also actively recruit behavioral health clinicians, help patients navigate the system to ensure care coordination, and monitor the availability of appointments and help members get appointments when needed,” the representative added — but stopped short of saying it was the AHIP’s responsibility to do so.
According to Caitlin Gillooley, senior associate director for policy at the American Hospital Association, “there has been some progress on the national landscape in improving parity law compliance, but its hard for the insurers themselves to quantify what it is they are covering.”
However, “ the nature of behavioral health care makes it a challenge,” she added.

Kennedy told Yahoo Finance that the government needs to invest more into mental health, and mental health compliance.
Even though the opioid crisis spurred thousands of lawsuits that could net states as much as $50 billion once it’s all over, the former congressman argued it only punishes the pharmaceutical sector.
“Why should it be that the pharmaceutical industry, which was rightfully held accountable for starting this fire, why should their dollars go to plugging the hole in treatment that is a result of the insurance industry not meeting their obligation,” Kennedy asked.
‘Traditional and longstanding barriers’
The stigma of behavioral health has started peeling away with the rise of the opioid crisis. leading to increased demand of behavioral health services. However, the problem is still pervasive.
Though hospitals were not included as part of the study, the AHA has been watching the trends within its membership nationwide. Earlier this year, the organization issued a report which highlighted the strategies hospitals are employing to improve care.
“Traditional and longstanding barriers to behavioral health access – such as lack of coverage and inadequate reimbursement – remain challenges for hospitals, health systems and patients,” the report said.
The issue is going mainstream in pop culture as well, as exemplified in the movie “Joker” and in a recent segment by comedian Hasan Minhaj on “Patriot Act,” his show on streaming platform Netflix (NFLX).
“If you thought insurance was bad about regular health care, they’re even worse about mental health care,” Minhaj said in the segment.
Telehealth has been seen as an inexpensive placeholder for behavioral health needs, and many telehealth programs work directly with employers to provide care. But that is not a replacement for an in-person visit, according to the AHA’s Gillooley.
She said that while hospitals are trying to find more partners— such as community behavioral health networks— there also needs to be more policy to help enforce the parity law and ensure stronger networks for coverage.
Anjalee Khemlani is a reporter at Yahoo Finance. Follow her on Twitter: @AnjKhem
Read the latest financial and business news from Yahoo Finance
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, SmartNews, LinkedIn, YouTube, and reddit.

 Yahoo Finance
Yahoo Finance 